
John Muthii Muriuki, Kenya Medical Research Institute
A deficiency of iron for normal body function is the most common nutritional disorder in the world. Iron deficiency is the main cause of anaemia and is associated with poor brain development and long-term impairment of behavioural and cognitive performance in children.
Common symptoms of iron deficiency include pallor of the skin, eye and beds of nails, weakness, difficulty breathing, dizziness, headache, hair loss, dry or rough skin and cravings for non-food items such as ice, paper, dirt, or clay.
Iron deficiency is commonly diagnosed using laboratory blood tests that mainly measure levels of ferritin, a protein that stores iron. In Africa, the tests can be misleading because ferritin levels go up in a person’s body during inflammation or infections such as malaria. This means that a person who is iron deficient may appear iron replete if they’re carrying an infection.
It is therefore challenging to estimate the burden of iron deficiency in settings such as sub-Saharan African where infections are common.
But accurate estimates of the burden of iron deficiency are important for designing public health interventions dealing with nutritional iron levels. Giving iron supplements based on poor data can lead to the wrong children being targeted. This could include children who should be getting supplements but aren’t, and those who don’t need them being given supplements with possible adverse effects.
To help overcome this problem we set out to calculate more reliable estimates of the burden of iron deficiency in African children.
Our study highlighted that a huge burden of iron deficiency may be missed out given the current tools used to measure it. This is important for governments to properly plan, monitor, and target effective interventions to deal with iron deficiency on the continent.
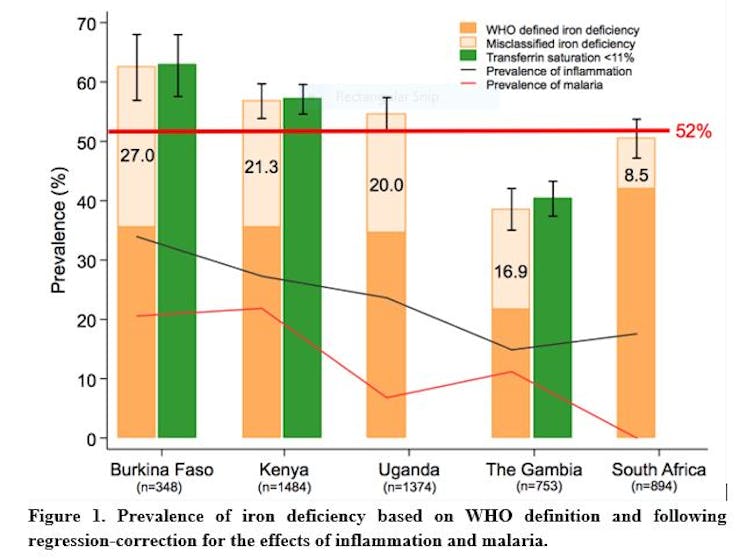
We analysed data for 4,853 children from communities in Kenya, Uganda, South Africa, Burkina Faso and The Gambia. We used statistical modelling to correct for the effects of malaria and inflammation on iron biomarkers. We found that over half (52%) of the African children were iron deficient.
We also found that transferrin saturation, an indicator of transferrin-bound iron in the bloodstream, may more accurately estimate the burden of iron deficiency in African children. This is because transferrin saturation was the iron biomarker least influenced by infections. We found that transferrin saturation below 11% may indicate iron deficiency in African children. Transferrin saturation is easy to measure in routine laboratory tests.
The implications
We found that ferritin levels may be elevated even before children are defined as having inflammation. We also found that malaria infection influenced ferritin levels independently of inflammation.
The influence of malaria infection on ferritin levels is not accounted for in the World Health Organisation’s definition of iron deficiency. In addition, its definition of iron deficiency accounts for the effect of inflammation by applying an arbitrary higher cut-off of ferritin levels in individuals with inflammation.
Using the World Health Organisation definition, the overall prevalence of iron deficiency was 34%. But this is an underestimate of the burden of iron deficiency (52%) that we found.
In some communities, where the prevalence of infections was high, over a quarter of the children were misclassified as iron replete whereas they were iron deficient.
This has huge implications for the rollout of nutritional iron programmes. The World Health Organisation uses the prevalence of anaemia as a proxy of iron deficiency or need in a population. The organisation recommends that daily iron supplementation should be provided to all children if the prevalence of anaemia is more than 40%. In places where malaria is prevalent, the iron supplementation should be provided in conjunction with effective malaria controls and treatment measures since giving iron may increase the risk of malaria infection.
In our study populations, the prevalence of anaemia was more than 40%. Therefore, based on the World Health Organisation recommendations, all children would receive iron supplementation although we found that approximately half of the children were iron deficient. Half of the children would needlessly take iron supplements. This suggests that the prevalence of anaemia is a poor indicator of iron need.
Giving iron supplements to children who are not iron deficient may predispose them to infections, including malaria. A large study in Pemba, Tanzania, showed that iron supplemented children were more likely to die or be admitted to hospital. In that study, iron supplementation increased the risk of malaria-related events by 16%. However, in iron deficient children, iron supplementation was not harmful.
How to manage iron deficiency
There are multiple causes of iron deficiency in children. These can include eating diets low in iron, impaired absorption of iron, excessive loss of iron through injury, increased iron need for growth, or genetic factors.
Iron in foods such as meat, fish and poultry is easily absorbed while iron found in plant foods, such as vegetables, cereals, beans and lentils, is poorly absorbed. Eating fruits rich in vitamin C enhances iron absorption. Grains and tea contain substances that inhibit iron absorption.
The need for iron varies. For example, iron requirements increase during the first year of a child’s growth. This means that weaning children should be supplemented with foods rich in iron.
In sub-Saharan Africa, chronic infections such as malaria, HIV, and TB are common. These diseases may be an underlying cause of iron deficiency. This is because they can cause a blockade of dietary iron absorption. Thus, even iron supplements may not be effectively absorbed in the presence of infections. The fortification of foods has also been associated with gut disorders since unabsorbed iron favours the growth of bad bacteria.
What this shows is that managing iron deficiency is complex and an integrated approach is required. Our study suggests that improved control of malaria and other infections would also improve assessment of iron status in African children.
Improved control of infections may also improve absorption of iron although future research should quantify the benefits of such an approach in addressing iron deficiency.
John Muthii Muriuki, PhD Fellow, Open University (UK), Kenya Medical Research Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.

