Shirin Moossavi, University of Calgary and Marie-Claire Arrieta, University of Calgary
The risk of severe COVID-19 infection is more common in those with high blood pressure, diabetes and obesity, conditions that are all associated with changes to the composition of the gut microbiome — the community of bacteria, viruses and fungi that live in the intestines. This raises the question of whether the gut microbiome has a role in dictating COVID-19 severity.
Let’s recap what we know about COVID-19. COVID-19 is a new disease caused by a very contagious virus called SARS-CoV-2.
In most infected individuals, the virus does not cause serious illness. However, it causes a very serious respiratory disease — and even death — in a minority of patients. Through many studies of people with COVID-19 over the past few months, we have learned what characteristics are more likely to be linked to mild versus severe forms of the disease.
Who is predisposed to serious COVID-19?
Children and young adults are less likely to develop symptomatic COVID-19, although infection readily occurs in young people with equally high viral loads in the airway, suggesting that they can certainly infect others. In contrast, people of older age and those with pre-existing chronic conditions are highly at risk and very likely develop symptomatic, severe disease.
If we consider the gradient of severity of the disease, children are at one end, and the elderly and patients with chronic conditions are at the other end.
What conditions are linked to severe COVID-19?
The information collected by researchers from many countries all points to similar characteristics and health conditions that are more commonly seen in patients with severe disease. These include older age, high blood pressure, diabetes and obesity.
The strength of these associations is even more prominent among younger individuals, as younger patients with obesity and diabetes are more likely to have serious disease.
In New York City, 5,279 patients tested positive for COVID-19 between March 1 and April 8, 2020. Of these, 22.6 per cent had diabetes and 35.3 per cent were obese.
Obesity was associated with an increased rate of hospital admission and critical illness. Similar findings were provided by investigators in the United Kingdom about the outbreak in Britain, where obese patients were twice as likely to develop severe disease.
Do these findings raise the possibility that the mechanisms underlying high blood pressure, diabetes and obesity may help explain why these conditions lead to severe COVID-19 disease? Before exploring this question, let’s zoom in on cellular and molecular mechanisms known to be involved in COVID-19 disease.
How does the body fight COVID-19 infection?
When the virus enters the body, it mostly goes to the airways and the gastrointestinal tract. The virus then binds to specific receptors present on the surface of epithelial cells to enter these cells. Viral replication within the cells leads to cell damage and cell death. This results in the release of specific signalling molecules that alert the local immune system.
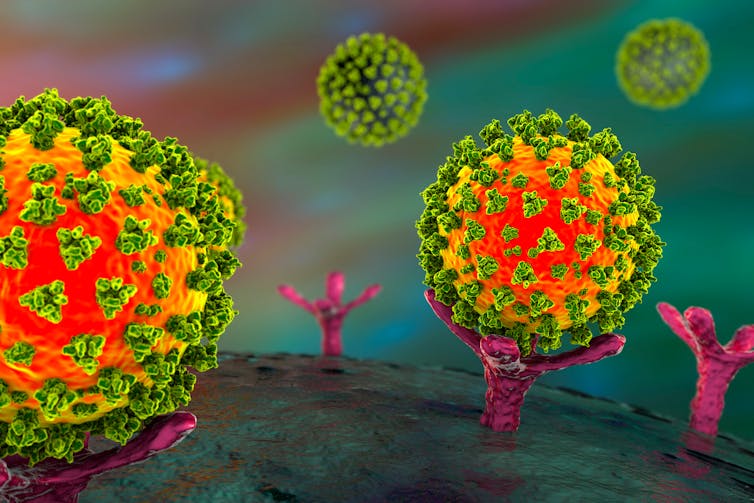
Armies of immune cells are then dispatched to initiate an antiviral response. Some of these cells are specialized to locate and identify the virus, while others mount a specific immune attack. The immune response results in the release of cytokines, chemokines and antibodies, which in many cases can defeat the virus, and the patient recovers.
Sometimes the immune system is dangerously at high alert and overreacts. In this case, the immune cells mount an especially strong inflammatory response — one that goes beyond what is required to kill the virus. This extra-strong attack releases cytokines and chemokines on a massive scale throughout the body, resulting in a cytokine storm, which causes widespread inflammation and tissue damage in patients with severe COVID-19.
One of the reasons for an abnormal, overreactive immune response lies in the gastrointestinal tract. Millions of interactions are constantly occurring between the immune system and trillions of non-dangerous microbes that live within the body. These interactions educate the immune system in how to function and, importantly, in how not to overreact to infectious microbes. Could this help explain why some people are more likely to develop uncontrolled inflammation upon COVID-19 infection?
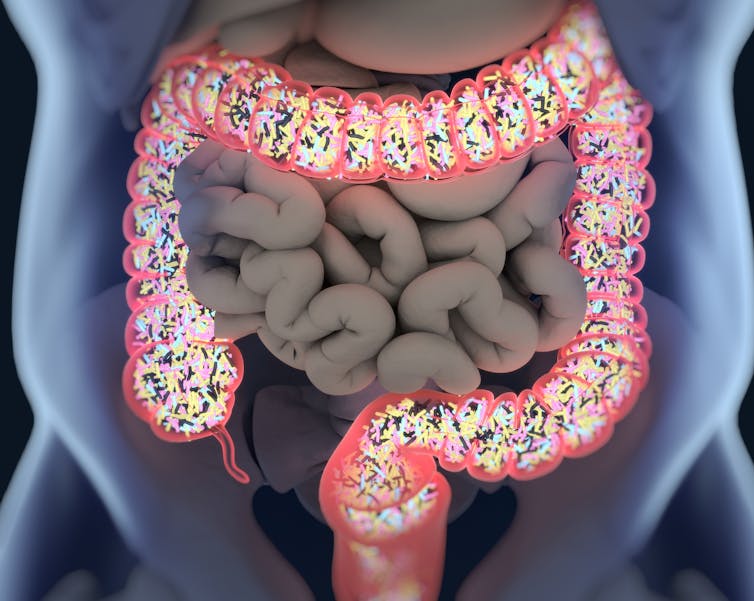
Trillions of micro-organisms that call your gastrointestinal tract home
The gut microbiome is the community of micro-organisms living inside the gastrointestinal tract, mostly in the large bowel. The microbiome contains bacteria, fungi (yeast), viruses and protozoa, all of which contribute to maintaining a balanced ecosystem and human health. These microbes collectively perform many beneficial functions, including educating the immune system.
When studying the microbiome, scientists examine the composition (what is there) and function (what are they doing) of this ecosystem. We have learned that both composition and function of the gut microbiome are important features linked to human health. In certain conditions, the balance of the gut microbiome composition and function is disrupted in a way that leads to disease, a phenomenon called microbiome dysbiosis.
There is accumulating evidence from animal and human studies that gut microbiome dysbiosis has a causal role in metabolism dysregulation manifested as diabetes and obesity — the risk factors of severe COVID-19 disease.
Is gut microbiome predisposing patients to severe COVID-19?
The gut microbiome regulates host defences against viral infections including respiratory viruses, such as influenza virus. This occurs through the activation of immune antiviral mechanisms and the prevention of excessive inflammation.
Different species of the gut microbiome have pro- or anti-inflammatory properties and play different roles in regulating the immune system. In the context of COVID-19, a recent preprint study (not yet peer reviewed) showed that specific members of the gut microbiome were associated with severe disease and with immune markers known to be elevated in severe disease. The association of these gut bacteria with the immune markers was even higher than that of the known risk factors of COVID-19 severity: age and obesity.
Further work is needed to confirm that pro-inflammatory microbial species can contribute to the immune responses that make severe COVID-19 more likely, but based on what we know about the microbiome, this is certainly a possibility. This also could mean that beneficial gut microbiome species, the type that promote low inflammation, have the potential to prevent or remediate the immune alterations that lead to severe COVID-19.
Potential for treatments and prevention
The research community is working very hard to develop and test safe and effective vaccines and treatments against COVID-19. Tapping into the potential of the gut microbiome is another avenue that we can pursue to identify potential safe and affordable probiotics for prevention and treatment. This is not unprecedented in the context of viral respiratory diseases: probiotics and prebiotics can affect the immune response to the flu vaccine, and may improve outcomes in flu-like illnesses.
Until effective treatments are available, “mind your microbes” and maintain a healthy lifestyle.
Shirin Moossavi, Postdoctoral Fellow, International Microbiome Centre, University of Calgary and Marie-Claire Arrieta, Assistant Professor, Physiology, Pharmacology and Pediatrics, University of Calgary
This article is republished from The Conversation under a Creative Commons license. Read the original article.

