
Gabriel Wainer, Carleton University and Hoda Khalil, Carleton University
The COVID-19 pandemic has taken its toll on everyone and we are all looking forward to getting back to normal. But an ill-planned return could result in new COVID-19 waves, which means more stay-at-home orders and further economic decline and mental stress challenges.
This is exacerbated by the appearance of new variants of concern, which are more infectious. Recent reports showed that the Delta and Kappa variants, which originated in India, can be transmitted in seconds by simply walking next to an infected individual.
Planning the smooth resumption of indoor activities under current circumstances can be challenging because there are many factors involved in ensuring a safe return. Ventilation in schools needs to be improved before kids return to class and safety measures must be tested and followed.
Safe return to normal
Some measures for guaranteeing a safe return to normal have already been taken, like providing vaccines to everyone. The COVID-19 vaccine provides considerably more protection than natural immunity and is more than 90 per cent effective at preventing hospitalization for older adults.
So far, there have been no guarantees that school children will be fully vaccinated before going back to school. More data is expected about the effect of vaccines on children between five and under 12 years of age, possibly after schools start. However, data for kindergarten children is not expected to be available at that time.
Other measures need to be taken to ensure the safety of schoolchildren before that time.
Safe schools
Measures such as physical distancing, proper ventilation and well-fitted face masks can substantially lower infection risks, if done properly.
Respirators like N95 and FFP are more effective than single-layer or surgical masks. The risk is much higher for health-care professionals and recent studies recommend that patients wear masks and first responders and medical experts respirators. Germany and other EU countries have mandated wearing respirators in public areas.
The effects of these interventions cannot be studied through experimentation because they compromise individuals’ health. Our research attempts to solve this problem through modelling and simulating the spread of the disease, particularly in indoor spaces in the built environment. Combined with data collection, our simulation models can help plan the safe return to campuses, offices, schools and stores.
The recipe to minimize the risks and create stronger plans can be summarized in three steps. The first step is finding affordable ways to measure indoor infection risks. Second, studying the factors that may elevate or reduce such risks using modelling and simulation. Finally, based on the results of the first two steps, visualizing how to mitigate the infection risks by controlling indoor environmental factors.
Step 1: Measure the risk of infection
There have been delays in recognizing that SARS-CoV-2 is airborne. Airborne viruses are spread through infectious aerosols and ballistic droplets that are emitted by people when they breathe, which can then be inhaled by another person.
The risk of inhaling virus-laden air depends on many factors including proximity, air direction and air exchange rate. And the risk of infection depends on both the amount of virus-laden air you breathe and the amount and type of virus present.
As a general rule, the risk of contracting airborne transmitted diseases indoors is high. There are numerous cases that show that aerosols in poorly ventilated indoor environments combined with superspreader events are the main cause for the spread of the disease.
Read more: Improving building ventilation can help us control the spread of COVID-19 during the winter months
Recent studies show outbreaks in a poorly ventilated courtroom and in various multi-unit buildings. There is increased risk for group living environments, which produced a higher number of secondary transmissions.
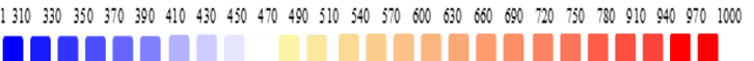
To study infection, we use carbon dioxide (CO2) as a proxy: higher CO2 concentrations in a space with infected occupants can be an indication that individuals are inhaling larger amounts of viral particles.
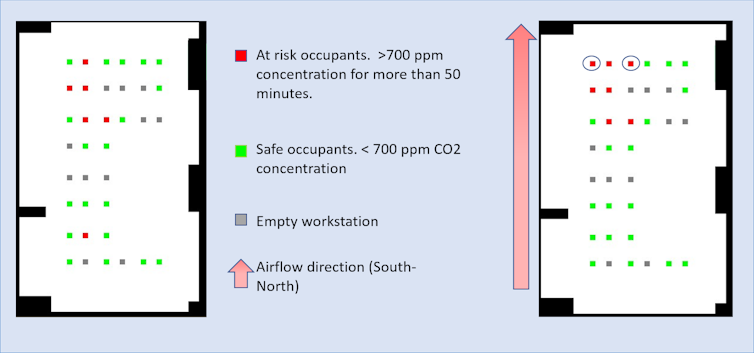
CO2 concentration can be easily measured using affordable sensors. Research has provided guidelines for safe indoor CO2 concentration levels that reduce indoor infection risk. The threshold of safe indoor CO2 concentration depends on occupants’ activity levels, for example sitting at a desk or exercising.
Detailed indoor guides show that the two-metre/six-foot rule is not enough to prevent contagion. Plastic barriers are also not always useful and may not result in lower transmission rates.
Step 2: Use simulations to conduct experiments
We created indoor CO2 dispersion models that mimic physical spaces while considering configuration factors that affect CO2 concentration. These factors include CO2 sources (occupants), CO2 sinks (windows and ventilation ports) and spatial dimensions. By comparing data collected from physical spaces and data collected from simulations of these spaces, our research proved that the models mimic reality to a great extent.
We have used a variation of the models to predict the risk of infection indoors, and have shown how different factors affect infection risks.
Measures should be in place to guarantee a healthy indoor environment before attempting to resume indoor activities at full capacity. Our simulation models show that considering simple measures — like opening windows — would help improve air quality and reduce the risk of infection indoors.
Poor ventilation would increase the CO2 concentration and consequently the risk of viral infection in the presence of sick occupants. Comparing poorly ventilated spaces to well-ventilated ones through a simulation, with exact configurations and seating arrangements, proves that providing well-ventilated spaces is a must before returning to schools and offices.
Step 3: Plan ahead
These indoor models provide a way to factor in and measure the effects of adjusting different configurations as needed.
Our research on simulating indoor CO2 spread is an example of how science and technology can provide affordable tools to support decision-makers. The next step is to apply these recommendations to make well-informed decisions for reopening schools and offices.
These recommendations include wearing high-quality masks that fit snugly against your face, high-quality ventilation and good air and temperature control to guarantee a safer return.
The simulation results can also be used to influence human behavior by providing positive messaging to help combat pandemic fatigue.![]()
Gabriel Wainer, Professor, Systems and Computer Engineering, Carleton University and Hoda Khalil, Postdoctoral fellow, Systems and Computer Engineering, Carleton University
This article is republished from The Conversation under a Creative Commons license. Read the original article.

