Matthew Quaife, London School of Hygiene & Tropical Medicine and Finn McQuaid, London School of Hygiene & Tropical Medicine
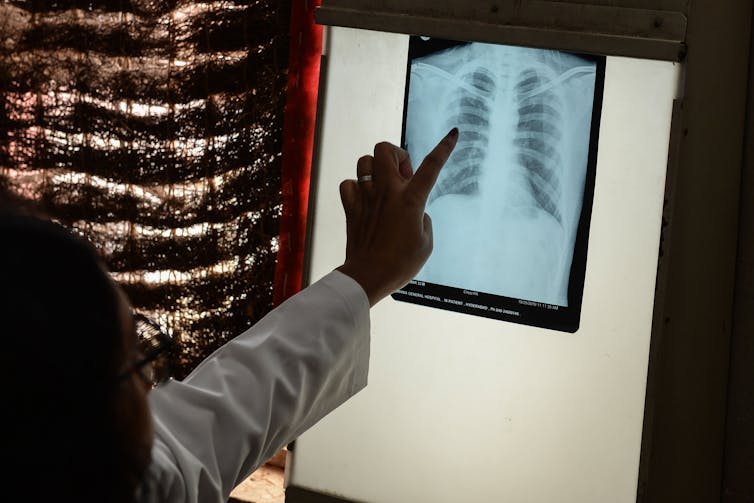
Two years of battling COVID-19 has been bad news for tuberculosis (TB) programmes. Respiratory clinicians and researchers have had their time and focus directed elsewhere. And TB has taken advantage. In 2021, the number of TB deaths rose for the first time in over a decade.
The barriers caused by lockdowns and overstretched healthcare systems have had a negative impact on TB diagnosis and treatment. The World Health Organisation found that 21% fewer people received care for TB in 2020 compared to 2019. Prevention, referral, and treatment programmes have all been heavily affected. To make matters worse, potential increases in poverty, undernutrition, and long-term lung damage due to COVID-19 are all likely to make many more people vulnerable to TB disease, which also causes significant long-term lung issues.
Despite COVID-19 disruptions, the world continues to work towards ambitious Sustainable Development Goal targets for 2030. The aim is to reduce TB deaths by 90%, cut new cases by 80%, and to ensure nobody faces catastrophic expenses due to TB. With just eight years to go, it is becoming increasingly clear that we are not on track to meet them. In fact, without game-changing tools to prevent more TB cases and deaths, we will be a long way off.
Hopes are pinned on new vaccines to be the game changers in reducing cases and deaths. Until now, the Bacille Calmette–Guérin (BCG) vaccine has been the only licensed vaccine against tuberculosis. But BCG protection does not last against pulmonary TB in adulthood, and because TB disease often occurs years after someone is first infected with TB bacteria, a vaccine which prevents severe TB disease after childhood is needed.
In 2019, the new M72/AS01E vaccine caused excitement in the TB field when a trial suggested it was 50% efficacious in preventing TB disease in sub-Saharan Africa. These exciting initial results need to be confirmed in a bigger trial. The pharmaceutical company GSK has licensed the vaccine to the Bill and Melinda Gates Medical Research Institute to lead its further development.
In the meantime, it’s vital for policymakers to understand whether this new vaccine will reduce deaths and ill-health from TB disease, and particularly whether it will be good value for money in the places where it’s needed.
This was the catalyst for our new modelling study in the London School of Hygiene and Tropical Medicine’s TB modelling group. We estimated the potential health impact and cost-effectiveness of the M72/AS01E vaccine in two high burden TB countries: India and South Africa.
Our findings suggest that the M72/AS01E vaccine could be a very good investment for vaccine developers and health systems, particularly if it is shown to offer protection among TB-uninfected people.
Potential impact
There is uncertainty about how the M72/AS01E vaccine will work, so we modelled two vaccine scenarios.
In the first scenario, 80% of adolescents were vaccinated at ages 12 or 15. In the second, 50% were vaccinated at 18 years old – reflecting anticipated challenges in reaching this older group, for example if they have left education. In the first scenario vaccines prevented TB disease, irrespective of whether the recipient was infected by TB bacteria when they were vaccinated. In the second, vaccines were effective only if the recipient was infected by TB bacteria at vaccination.
We found that routine vaccination of adolescents could have a huge health impact and be cost-effective in reducing TB deaths and disease. Vaccinating adolescents is key to protect people at the ages when TB is most common.
In South Africa, all vaccination scenarios modelled in all age groups were highly cost-effective. We assessed this by analysing how much each vaccine scenario cost to prevent one disability-adjusted life year (DALY), a measure which captures quality and quantity of life saved. There was a 94-100% probability they had a lower cost per DALY averted than a threshold representing good value-for-money. Most became cost-saving when we accounted for the fact that vaccines also prevent patients incurring considerable costs when accessing TB care.
In India, a vaccine modelled to prevent TB disease regardless of whether someone is already infected with TB bacteria was also highly cost-effective. There was a 92-100% probability of lower cost per DALY averted than the threshold. A vaccine which only protects against progression to TB disease when someone is already infected with TB bacteria was unlikely to be cost-effective (0-6% probability of cost-effectiveness).
So far, the evidence on M72/AS01E efficacy from the trial was only for people previously infected with TB bacteria. It is hoped that efficacy will also be high among people before infection with TB bacteria. But it is likely to be many years before we know whether this is true or not, in part because trials need a huge number of participants.
Learning from COVID-19
It is critical to learn from the successes and failures of COVID-19 vaccines.
In countries such as the UK, population-wide COVID-19 vaccination has happened much quicker than anyone working in public health could have dreamt of before the pandemic. Yet in many settings, particularly those most affected by TB, COVID vaccination coverage remains poor. The situation is even worse in the communities most affected by TB.
It is therefore critical to prepare the ground for introducing these vaccines. The first step is speaking to communities and people who will receive them to understand how vaccines can be introduced in a way which meets their needs and preferences.
It’s clearer than ever that continued investment in prevention and care is needed to reach the End-TB goals. Vaccines like M72/AS01E, and other candidates in the pipeline, are likely to be key in the battle to reduce death and disability caused by TB.![]()
Matthew Quaife, Assistant Professor in Health Economics, London School of Hygiene & Tropical Medicine and Finn McQuaid, Assistant Professor, Infectious Disease Epidemiology , London School of Hygiene & Tropical Medicine
This article is republished from The Conversation under a Creative Commons license. Read the original article.

