Our brain is an extremely complex and delicate organ. Our body fiercely protects it by holding onto things that help it and keeping harmful things out, such as bugs that can cause infection and toxins.
It does that though a protective layer called the blood-brain barrier. Here’s how it works, and what it means for drug design.
First, let’s look at the circulatory system
Adults have roughly 30 trillion cells in their body. Every cell needs a variety of nutrients and oxygen, and they produce waste, which needs to be taken away.
Our circulatory system provides this service, delivering nutrients and removing waste.
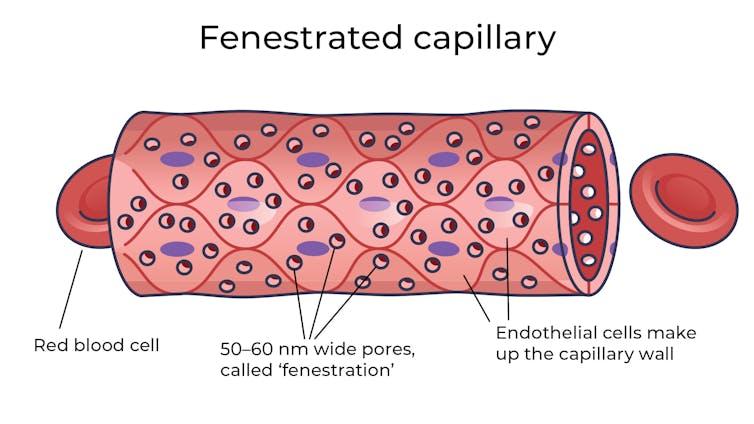
Where the circulatory system meets your cells, it branches down to tiny tubes called capillaries. These tiny tubes, about one-tenth the width of a human hair, are also made of cells.
But in most capillaries, there are some special features (known as fenestrations) that allow relatively free exchange of nutrients and waste between the blood and the cells of your tissues.
It’s kind of like pizza delivery
One way to think about the way the circulation works is like a pizza delivery person in a big city. On the really big roads (vessels) there are walls and you can’t walk up to the door of the house and pass someone the pizza.
But once you get down to the little suburban streets (capillaries), the design of the streets means you can stop, get off your scooter and walk up to the door to deliver the pizza (nutrients).
We often think of the brain as a spongy mass without much blood in it. In reality, the average brain has about 600 kilometres of blood vessels.
The difference between the capillaries in most of the brain and those elsewhere is that these capillaries are made of specialised cells that are very tightly joined together and limit the free exchange of anything dissolved in your blood. These are sometimes called continuous capillaries.
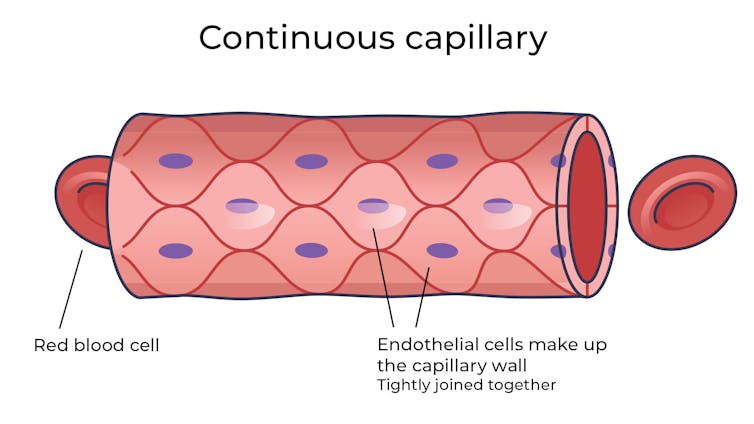
This is the blood brain barrier. It’s not so much a bag around your brain stopping things from getting in and out but more like walls on all the streets, even the very small ones.
The only way pizza can get in is through special slots and these are just the right shape for the pizza box.
The blood brain barrier is set up so there are specialised transporters (like pizza box slots) for all the required nutrients. So mostly, the only things that can get in are things that there are transporters for or things that look very similar (on a molecular scale).
The analogy does fall down a little bit because the pizza box slot applies to nutrients that dissolve in water. Things that are highly soluble in fat can often bypass the slots in the wall.
Why do we have a blood-brain barrier?
The blood brain barrier is thought to exist for a few reasons.
First, it protects the brain from toxins you might eat (think chemicals that plants make) and viruses that often can infect the rest of your body but usually don’t make it to your brain.
It also provides protection by tightly regulating the movement of nutrients and waste in and out, providing a more stable environment than in the rest of the body.
Lastly, it serves to regulate passage of immune cells, preventing unnecessary inflammation which could damage cells in the brain.
What it means for medicines
One consequence of this tight regulation across the blood brain barrier is that if you want a medicine that gets to the brain, you need to consider how it will get in.
There are a few approaches. Highly fat-soluble molecules can often pass into the brain, so you might design your drug so it is a bit greasy.

Another option is to link your medicine to another molecule that is normally taken up into the brain so it can hitch a ride, or a “pro-drug”, which looks like a molecule that is normally transported.
Using it to our advantage
You can also take advantage of the blood brain barrier.
Opioids used for pain relief often cause constipation. They do this because their target (opioid receptors) are also present in the nervous system of the intestines, where they act to slow movement of the intestinal contents.
Imodium (Loperamide), which is used to treat diarrhoea, is actually an opioid, but it has been specifically designed so it can’t cross the blood brain barrier.
This design means it can act on opioid receptors in the gastrointestinal tract, slowing down the movement of contents, but does not act on brain opioid receptors.
In contrast to Imodium, Ozempic and Victoza (originally designed for type 2 diabetes, but now popular for weight-loss) both have a long fat attached, to improve the length of time they stay in the body.
A consequence of having this long fat attached is that they can cross the blood-brain barrier, where they act to suppress appetite. This is part of the reason they are so effective as weight-loss drugs.
So while the blood brain barrier is important for protecting the brain it presents both a challenge and an opportunity for development of new medicines.![]()
Sebastian Furness, ARC Future Fellow, School of Biomedical Sciences, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.

