
Michael Plank, University of Canterbury; Andrew Sporle; Kate Hannah; Melissa McLeod, University of Otago, and Nicholas Steyn
The risk of dying from COVID-19 is at least 50% higher for Māori than New Zealanders from European backgrounds, according to our study published today.
Māori and Pacific populations are historically at greater risk of hospitalisation and death from pandemics. During the 2009 influenza pandemic, the rate of infection for Māori was twice that of Pākehā (European New Zealanders). Māori were three times more likely to be hospitalised and almost three times more likely to die.
Our results show that if COVID-19 were allowed to become more widespread in New Zealand, it would have a devastating impact on Māori and Pacific communities.
Higher risks for Māori and Pacific people
Evidence from overseas shows ethnic minority communities are at greater risk of serious health problems from COVID-19. In some parts of the US, Pacific islanders are being hospitalised at up to ten times the rate of other ethnicities. In the UK, Black and minority ethnic groups are suffering death rates twice those of White people.
Read more: Why are black and Asian people at greater risk of coronavirus? Here's what we found
Our study was based on international data on risk factors for COVID-19 fatality, including heart disease, diabetes and asthma. We combined these with data on the prevalence of these conditions in different ethnic and age groups in New Zealand.
We also accounted for the fact that Māori and Pacific people have lower life expectancy and higher unmet health-care needs than European New Zealanders.
We found the risk of death from COVID-19 was at least 50% higher for Māori. It could be more than double the rate for European New Zealanders if the level of unmet healthcare need is actually greater than official data can capture. The risk for Pacific people could also be up to double that for European New Zealanders.
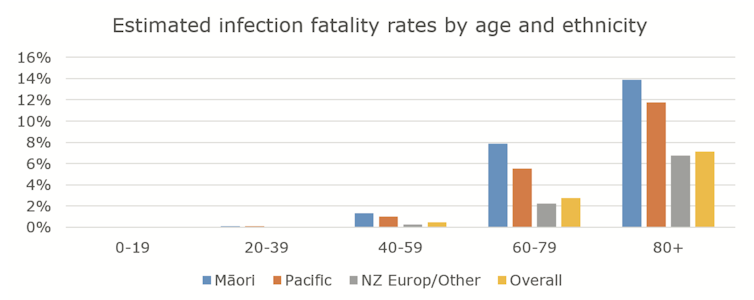
One of the immediate reasons for the higher risk Māori and Pacific people face is that they have higher rates of existing health conditions. These are strongly associated with more severe outcomes from COVID-19.
Māori and Pacific populations are younger, on average, than Pākehā. But they have lower life expectancy and tend to experience health issues at a younger age. They also experience greater rates of unmet healthcare need and greater levels of poverty, which have been shown to have a significant effect on fatality rates.
For these reasons, Māori and Pacific people are also at higher risk of becoming severely ill and needing to go to hospital as a result of COVID-19. Unfortunately we are now starting to see this happen. COVID-19 cases among Māori and Pacific people have been around twice as likely as other ethnic groups to require hospitalisation.
Read more: Two inquiries find unfair treatment and healthcare for Māori. This is how we fix it
Substandard housing contributes to higher risk
Our study looked at the risk of death only once someone has become infected with COVID-19. But there are other factors that increase the risk of getting infected for Māori and Pacific people.
A recent study from the UK showed infection rates were much higher for people living in a large household or in poorer areas, while the epidemic in China indicated that around 80% of community transmission resulted from households.
About 25% of Māori and 45% of Pacific people live in crowded housing. They are also more likely to work in jobs or workplaces with higher health risks, including infection.
COVID-19 would therefore be a double whammy for these communities: a higher rate of infection and a higher risk of severe illness or death following infection.
Implications for COVID-19 response
These findings show the potentially devastating impact COVID-19 could have on Māori and Pacific communities in New Zealand. The pandemic has potential to intensify existing social inequities that result from colonisation and systemic racism.
Our health-care system was under resource pressure prior to COVID-19 and was already being challenged for its inequitable care. The results of our study reinforce the importance of controlling the virus and preventing it from spreading into at-risk communities. It also highlights the need for measures that work well for affected communities to protect at-risk groups.
A “one size fits all” approach will result in higher rates of avoidable illness and death for Māori and Pacific communities. Te Rōpū Whakakaupapa Urutā, the National Māori Pandemic Group, has clearly argued that if New Zealand wants to prevent these outcomes, the pandemic response must focus on equity.
Routine monitoring and reporting of the impact of the pandemic needs to explicitly address equity. That will require an approach that supports communities to design and deliver interventions that are effective for them.![]()
Michael Plank, Professor in Mathematics, University of Canterbury; Andrew Sporle, Honorary Senior Research Fellow; Kate Hannah, Researcher; Melissa McLeod, Senior research fellow, University of Otago, and Nicholas Steyn, Research assistant
This article is republished from The Conversation under a Creative Commons license. Read the original article.

